VA PTSD Ratings Explained: How the VA Decides Your Disability in 2026
PTSD VA ratings are one of the most confusing and frustrating parts of the VA disability system.
Many veterans meet symptom criteria but still receive a lower rating, are misunderstood during C&P exams, or see others with similar symptoms awarded higher percentages.
If this sounds familiar, you are not alone. While PTSD ratings often seem inconsistent, the VA actually follows predictable patterns.
This guide explains how the VA decides PTSD ratings, common mistakes that lead to lower percentages, and how to strengthen your claim.
What is a VA Rating for PTSD?
In simple terms, a VA PTSD rating is a percentage the VA assigns to reflect how much PTSD affects a veteran’s ability to work and function socially.
Before the VA can assign a rating, the condition must be service connected. This requires three things: a verified in-service stressor, a current PTSD diagnosis from a qualified medical provider, and medical evidence linking the PTSD to that stressor.
A Current PTSD Diagnosis
The VA requires a formal PTSD diagnosis that meets DSM-5 diagnostic criteria from a qualified mental health provider, such as a psychiatrist, psychologist, or licensed clinician.
A PTSD rating cannot be granted without a current diagnosis, even if symptoms are severe.
A Verified In-Service Stressor
The veteran must show that a traumatic event occurred during military service.
Combat stressors: Traumatic events related directly to combat, such as enemy fire, explosions, or active combat operations. These are often easier for the VA to verify through service records or awards.
Non-combat stressors: Traumatic experiences outside of direct combat, such as military sexual trauma, serious accidents, training incidents, or other traumatic events during service.
While Non-combat stressors are legitimate causes of PTSD, you often need a medical opinion from a doctor linking your trauma to your condition.
A Medical Nexus Linking PTSD to Service
There must be medical evidence connecting the current PTSD diagnosis to the in-service stressor.
Built-in nexus: If your VA exam or medical records clearly states that PTSD is caused by or related to the in-service trauma, you’ve satisfied the nexus requirement
Missing nexus: This happens when PTSD is diagnosed but the records only list symptoms or a diagnosis without connecting it to the in-service event
If your nexus isn’t built in, you may want to consider getting a nexus letter for ptsd to link your condition to your time in service.
How VA Ratings for PTSD Actually Work
Once you are service connected for PTSD, the VA assigns a rating based on how much the condition impairs your ability to work and maintain relationships.
This is done by reviewing your symptom history and how those symptoms have impacted your ability to function.
How the VA Measures Work and Social Impairment
To determine a veteran’s level of impairment, the VA often looks at how PTSD affects their ability to work, maintain relationships, and manage daily life
The VA uses a holistic analysis, meaning it looks at the veteran’s average level of impairment over the long term.
They consider things like:
“whether the impairment is sustained over time”
“whether the veteran can maintain employment and relationships”
“whether impairment appears only during periods of stress or is more persistent”
After this, the VA reviews the veteran’s symptom history and how it connects to their overall level of impairment.
How the VA Evaluates Symptoms
At each level of impairment, the VA generally expects certain types of symptoms to be present.
The primary criteria they use include:
Frequency: How often symptoms interfere with work, relationships, or daily functioning.
Duration: How long those symptoms last when they occur.
Intensity: How severe the symptoms are when they happen.
In general, having more symptoms within a certain level can support a higher rating. However, this isn’t always the case, since the impact of symptoms can vary from veteran to veteran.
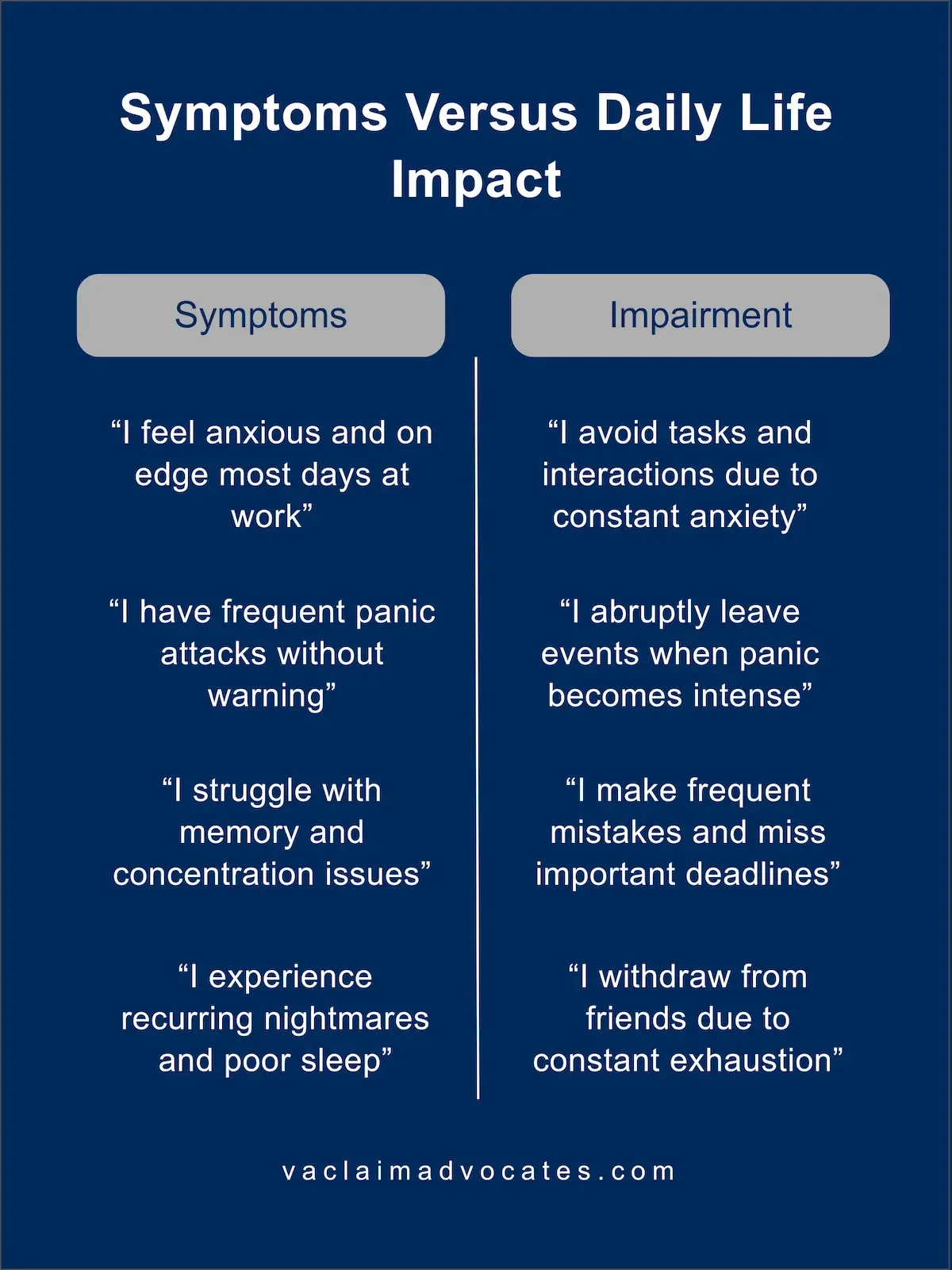
Why Two Veterans With Similar Symptoms Get Different Ratings
Often, two veterans can report very similar symptoms but receive different ratings because those symptoms affect their daily functioning in different ways.
For example, two veterans may both experience frequent panic attacks. One may still be able to work and manage daily tasks, while the other may miss work regularly or avoid leaving home because of them.
The difference is not whether symptoms exist, but how the VA evaluated their impact.
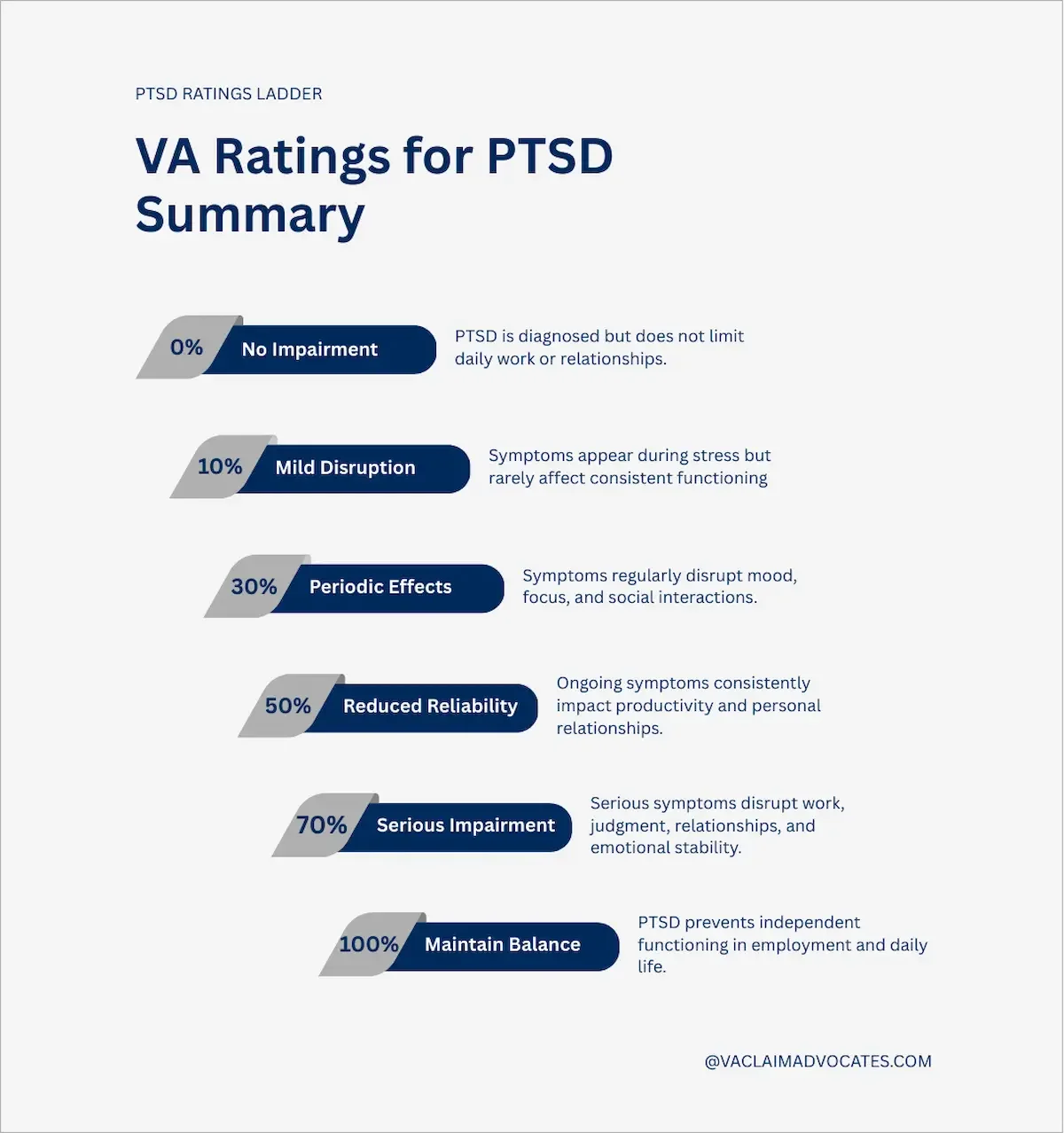
The VA PTSD Rating Chart From 0-100% Explained
Each PTSD rating reflects a veteran’s level of impairment and the types of symptoms commonly seen at that level.
While veterans usually show some of the symptoms listed for a rating level, they don’t need to match every symptom exactly to qualify for a specific rating.
PTSD is rated under VA Diagnostic Code 9411 within 38 CFR §4.130, which outlines the mental health rating criteria from 0% to 100%.
0% PTSD Rating — Service Connected With No Functional Impact
The VA assigns a 0% PTSD rating when a veteran has PTSD and is service connected, but the condition does not cause measurable social or occupational impairment.
Veterans with this rating typically:
have a PTSD diagnosis
are service connected for PTSD
are able to function normally at work and socially
Some veterans are incorrectly placed at 0% even though their symptoms do cause impairment. This does not mean the rating can never change. Later in this guide, we explain what to do if this applies to you.
10% PTSD Rating — Symptoms That Appear During Stress
Veterans at the 10% level usually experience symptoms that surface during periods of stress but do not consistently interfere with daily functioning.
This often looks like:
Occasional issues at work — Stressful or high-pressure situations may trigger symptoms
Infrequent panic attacks — Monthly or sporadic episodes are common
Mild sleep problems — Nightmares or waking during the night may occur at times
Veterans at this rating do experience PTSD symptoms, but they are generally able to function consistently at work and socially.
30% PTSD Rating — Ongoing Symptoms That Affect Daily Life
At the 30% level, veterans can still function overall, but symptoms begin to interfere more regularly with mood, thinking, and daily life.
Common examples include:
More difficulties at work — Memory issues, poor sleep, and concentration problems may affect performance
More frequent panic attacks — Symptoms become more noticeable and recurring
Reduced social engagement — Depression or anxiety may lead to isolation
The main difference between 10% and 30% is frequency and consistency. Symptoms are still relatively mild, but they appear more often and begin to affect functioning more regularly.
50% PTSD Rating — Symptoms That Regularly Disrupt Work and Relationships
At a 50% rating, symptoms are frequent and severe enough to consistently impact work performance and relationships.
This often includes:
Ongoing decrease in work performance — Cognitive issues, focus problems, and emotional symptoms regularly interfere with job duties
Frequent panic attacks — Often occurring weekly or more
Relationship difficulties — Veterans may still have relationships, but conflict, withdrawal, or trust issues are common
The main difference between 30% and 50% is the consistent decline in reliability and productivity, along with more severe symptoms that regularly disrupt daily life.
Need Help With Your VA Claim?
Speak with a VA claims specialist to understand your options and next steps.
Call 888-820-852070% PTSD Rating — Severe Problems in Most Areas of Life
Veterans at the 70% level experience serious impairment across most areas of life, including work, relationships, and emotional functioning.
This may include:
Suicidal ideation — This includes both passive thoughts and active intent, and is one of the strongest indicators of severe impairment
Major work difficulties — Frequent conflicts, poor performance, or repeated job loss
Severe relationship problems — Many veterans have very few relationships, and existing ones are often strained or broken
Not every symptom is required to qualify for a 70% rating. However, suicidal ideation is widely recognized as especially strong evidence at this level. This is discussed in more detail later.
100% PTSD Rating — Total Inability to Work or Function Socially
A 100% PTSD rating is reserved for veterans whose symptoms cause total impairment in both work and social functioning.
This often involves:
Inability to function socially — Basic communication and interaction may be extremely limited
Severe psychiatric symptoms — Such as hallucinations or severe disorganization of thought
Inability to manage daily life — Including neglect of personal hygiene or basic self-care
To qualify for a 100% rating, the VA must find that PTSD results in total occupational and social impairment. If a veteran is able to consistently work, maintain meaningful relationships, or function independently, the VA usually will not assign this rating.
How Much Does PTSD Disability Pay?
Once a PTSD rating is assigned, monthly compensation is based on that percentage and whether a veteran has dependents such as a spouse, children, or dependent parents. Rates are also adjusted each year for inflation.
Here is a simple snapshot of what PTSD ratings generally pay for a veteran with no dependents (as of 2026):
10% PTSD rating: around $180 per month
30% PTSD rating: around $500 to $600 per month
50% PTSD rating: around $1,000 to $1,100 per month
70% PTSD rating: around $2,000+ per month
100% PTSD rating: around $3,700+ per month
Veterans with dependents typically receive higher monthly amounts.
For exact and updated payment tables based on family status, the VA publishes full compensation rate charts each year.
New Rules for PTSD VA Compensation
The VA is working on an update to the VA Schedule for Rating Disabilities (VASRD), which would change how PTSD and other mental health conditions are evaluated.
These updates are still proposed and not yet in effect, and would also effect tinnitus ratings and sleep apnea ratings.
Key changes for PTSD include
Domain-Based Ratings — PTSD would be evaluated across specific functional areas such as thinking and memory, relationships, task completion, daily activities, and self-care instead of broad impairment categories.
Minimum 10% Mental Health Rating — The current 0% rating for mental health conditions would be removed, meaning any service-connected PTSD diagnosis would receive at least a 10% rating.
Clearer, More Objective Criteria — The VA would use more structured, measurable standards to guide examiners, which could reduce inconsistent ratings caused by vague or subjective exam language.
As of now, the VA continues to rate PTSD under the existing system based on severity, frequency, duration, and overall social and occupational impairment. No official effective date has been announced for these proposed changes.
How to Get a C&P Exam That Helps Your Rating
C&P exams play a major role in PTSD ratings because examiners document how impaired a veteran appears in the record. The VA relies heavily on the examiner’s judgment for this when assigning a rating.
What C&P Examiners Focus On When Evaluating PTSD
When evaluating a veteran during a C&P exam, examiners focus on a few core areas that help determine overall impairment.
These typically include:
Symptom timeline over the years: For each symptom, explain when it started, how long it has lasted, and whether it has worsened over time.
Work and relationship history: Be specific about job changes, terminations, divorces, or major relationship issues, including roughly when they occurred.
Consistent symptom patterns: Frequency matters. Examiners often note wording such as daily, weekly, or monthly to understand how regularly symptoms interfere with functioning.
I highly recommend writing out your timeline before the exam. Trying to remember important details on the spot is difficult and can lead to unclear information.
Focus On Your Worst Days in Detail
Describing what your worst days look like in detail is one of the best ways to help the examiner understand how PTSD truly affects your life.
Your worst days show:
How intense your symptoms become (severity)
How often those bad periods happen (frequency)
How long they last before you stabilize again (duration)
A lot of veterans are used to toughing it out and hiding how hard things really are, but this often makes symptoms appear way less severe during the exam.
Give Real Life Examples, Not General Impairments
Because a C&P examiner’s opinion depends heavily on how well they understand your condition, leaving out specific details can significantly weaken your claim.
To assign a PTSD rating, the VA needs to see clear examples of how symptoms measurably affect a veteran’s life, not just vague descriptions of impairment.
Vague example: PTSD makes me feel stressed sometimes.
Clear example: PTSD causes panic attacks one to two times per week, usually at work, which significantly reduce my ability to focus and complete tasks.
The more specifics you can give about the frequency and intensity of your symptoms, the easier it is for the VA to see impairments.
Avoid Mistakes that Lead to a Lower Rating
Many veterans are told that certain symptoms automatically qualify them for specific PTSD ratings.
While some symptoms can strongly support a higher rating, you still need to show how they contribute to impairment in concrete ways.
Examples:
Wrong: Listing every suicidal thought from the past year without explaining how it affects sleep, work, or daily functioning.
Right: Describing when suicidal thoughts usually occur and explaining how they make it difficult to sleep and concentrate at work each day.
Symptoms are still important, and you should clearly explain their frequency, severity, and duration. Just remember that symptoms are primarily evidence for impairment, not proof of impairment.
PTSD Rating Reductions, Reexams, & Risks Explained
PTSD ratings are not always permanent, and certain actions can trigger reexaminations or reductions.
Understanding when to seek an increase and when doing so may backfire can help veterans protect their existing rating.
When the VA Is Allowed to Lower a PTSD Rating
The VA cannot reduce a PTSD rating simply because it wants to. Reductions are only allowed under specific conditions.
Common situations where reductions may occur include:
Evidence shows sustained improvement: Medical records or exams must indicate real improvement over time, not just a temporary good period.
A new C&P exam suggests lower impairment: If an examiner documents significantly better functioning, the VA may propose a reduction.
Failure to attend a required reexamination: Missing a scheduled exam can sometimes trigger action on a rating.
In most cases, the VA must show clear and lasting improvement before lowering a PTSD rating.
A single good day or short-term improvement usually should not justify a reduction, but consistent documentation matters.
What a Proposed PTSD Reduction Notice Means
When the VA plans to reduce a PTSD rating, it usually sends a proposed reduction notice first.
This does not mean the rating has already been lowered.
A proposed reduction typically means:
the VA believes evidence suggests improvement
you have time to respond before any change happens
you can submit evidence to challenge the reduction
This type of review most commonly happens during a Higher-Level Review, when the VA takes a closer look at the full record. If your existing evidence is already weak or inconsistent, that closer review can sometimes lead to a proposed reduction.
Why Higher-Level Reviews Sometimes Backfire
Higher-Level Reviews are most risky when the foundation of the claim is not strong.
They are more likely to backfire when:
Service records are weak or unclear: There is limited documentation tying PTSD symptoms to service events.
Buddy or lay statements are missing or not detailed: There is little supporting evidence describing real-life impairment.
Symptoms have significantly improved since the original rating: In these cases, the VA may order a new C&P exam, which can document lower impairment and trigger a reduction.
Higher-Level Reviews should usually be filed only when your case has strong supporting evidence, the C&P exam is clearly flawed, and your symptoms have remained consistent since your original rating.
How to Increase Your PTSD Rating Safely
Safely increasing a PTSD rating requires understanding the strength of your evidence, whether a prior C&P exam was flawed, and how much impairment the next rating level requires. Higher ratings generally require stronger proof.
Show Long-Term Worsening Before Filing for an Increas
Before filing for a PTSD rating increase, your record should clearly show worsening symptoms that affect work and social functioning over time.
Useful documentation usually includes:
Recent mental health treatment notes describing functional problems such as missed work, conflicts, isolation, panic episodes, poor focus, or sleep disruption
Medication changes or ongoing therapy showing symptoms have persisted or worsened
A clear timeline of when symptoms worsened and how long the changes have lasted
Increase claims are often weak when there is little recent treatment evidence or when records repeatedly describe improvement or stability.
Actionable takeaway:
File for an increase only when recent records consistently show real impairment, not just the presence of symptoms.
Use Real-Life Evidence to Prove Impairment
Lay and buddy statements help show how PTSD affects daily life beyond medical appointments.
Strong statements usually include:
specific examples tied to work reliability and relationships
frequency language such as daily, weekly, or monthly
before-and-after comparisons
General statements without examples carry less weight.
Actionable takeaway:
Use statements to document observable changes and consistent functional problems, not just general struggles.
Fix Errors From a Bad C&P Exam
Because the VA heavily relies on C&P exams, an inaccurate report can block an increase or even trigger a reduction.
Common exam problems include:
important symptoms left out
severity described as mild when it is frequent or serious
timelines shortened or misstated
notes suggesting normal functioning despite ongoing work or social issues
When this happens, next steps usually depend on the situation:
Proposed reduction: respond within the deadline, request the hearing if offered, and submit evidence correcting the exam
Denied or low increase: use a supplemental claim to add new evidence, or an HLR only when the VA clearly misapplied existing evidence
If a C&P exam does not reflect your real impairment, address it quickly with corrections and supporting evidence before moving forward.
VA PTSD Rating Statistics
Real VA data helps show how PTSD ratings usually break down in practice. Here’s a quick look at how mental health claims are most often rated.
What is the Most Common PTSD Rating?
Based on recent VA data from 2024, about 2,837,602 mental health disability cases were processed. These include PTSD claims evaluated under the VA’s standard mental health rating system.
Of those cases, roughly 34.7% were rated at 70%, making it the most common PTSD-related rating level.
How Rare Is a 100% PTSD Rating?
Recent data shows that about 13.3% of PTSD cases receive a 100% rating.
While this data includes all mental health conditions, the VA uses the same rating criteria across mental health claims. Because of this, PTSD ratings tend to follow a similar distribution.
What Is the Average VA Rating for PTSD?
Based on recent mental health claims data, the average VA disability rating is approximately 56.5%.
Here’s how ratings are commonly distributed:
0% — 1.5%
10% — 3.5%
30% — 17.9%
50% — 26.4%
70% — 34.7%
100% — 13.3%
VA PTSD Rating Statistics (2024)
Based on 2024 VA mental health disability cases (about 2,837,602 processed). PTSD is rated under the same mental health criteria, so the distribution is a useful benchmark.
- Most common rating: 70% (about 34.7% of cases)
- How “rare” is 100%? About 13.3% of cases
- Average rating (approx.): 56.5%
Note: This is mental health claims data overall, but the VA applies the same general rating framework across mental health conditions, so PTSD outcomes often track closely.
Key Takeaways About VA PTSD Ratings
PTSD ratings are based on how symptoms consistently impact work and daily life, not on counting symptoms or focusing on diagnoses alone.
The VA looks at severity, frequency, and duration, with C&P exam language and medical records often carrying the most weight.
Many veterans receive confusing ratings because impairment is minimized or misunderstood, not because their condition is less serious.
Understanding how the VA evaluates PTSD can help veterans avoid common mistakes and strengthen their claims.
FAQ
-
One of the strongest ways to support a 70% PTSD rating is by showing suicidal ideation. Many veterans experience this more than they realize, and it can include passive thoughts, not just active plans or intent.
However, suicidal ideation is not required for a 70% rating. The main focus should be on demonstrating consistent, severe symptoms over time and clearly showing how those symptoms impact work and social functioning.
Buddy statements and lay statements can be especially helpful in documenting long-term impairment.
-
This is very common and usually comes down to how much the symptoms impair daily life. Two veterans can experience the same symptoms, but one may be able to function better at work or in relationships than the other.
How clearly symptoms are explained and documented during the C&P exam also plays a major role.
If impairment is not fully captured in the exam report, the VA may assign a lower rating even when symptoms are similar.
-
A 100% PTSD rating represents total occupational and social impairment. The VA is looking for near complete inability to function in both work and social environments.
If there are still parts of a veteran’s work life or social life that function in a meaningful way, the VA will usually determine that total impairment is not present and assign a lower rating
-
No. Mental health conditions are rated under one combined system by the VA. While a veteran can be service connected for multiple mental health diagnoses, separate ratings are not assigned when symptoms overlap.
In these cases, the VA uses a single rating that reflects the highest level of overall impairment.
-
No, PTSD ratings are not automatically permanent. The VA commonly schedules reexaminations every two to five years, especially when improvement is expected.
Keeping consistent treatment records and documenting ongoing symptoms can help protect a rating during future reviews.
-
Yes. Non-combat PTSD claims are just as valid as combat-related claims. PTSD can result from many types of traumatic experiences, not only combat.
The main challenge with non-combat claims is proving that the stressor event occurred and showing that it caused the PTSD.
-
No, being service connected for PTSD does not automatically guarantee a 50% rating.
This is because being service connected by itself doesn't automatically mean it impairs you to the criteria required for 50% which requires that your symptoms significantly disrupt relationships