Nexus Letters for PTSD: Most Veterans Are Doing It Wrong
There’s no shortage of confusing information about PTSD claims and nexus letters. Some veterans are told they must get one or they’ll be denied. Others get approved with no nexus letter at all — sometimes with high ratings.
That contradiction is what frustrates veterans the most.
The truth is this: not every PTSD claim needs a nexus letter, but when one is required, it has to be done the right way.
As a veteran who’s been through the VA claims process myself, I wrote this guide to explain:
How PTSD claims actually get approved
When a nexus letter helps & when it’s unnecessary
Exactly how to get a strong one if you need it.
This isn’t a sales pitch or legal theory. It’s a practical roadmap to giving your PTSD claim the best chance of approval.
Do You Actually Need a PTSD Nexus Letter for VA Service Connection?
To grant service connection for PTSD, the VA requires three things: a current PTSD diagnosis, evidence that an in-service stressor occurred, and a medical nexus linking that stressor to your PTSD.
In most cases, the nexus comes from the VA C&P exam, not a private doctor. A private nexus letter is usually only needed if the C&P examiner gives a negative opinion.
Even if you’re already service-connected for PTSD, you can often get a nexus letter for secondary conditions. This article, however, will focus on direct connections.
The 3 Things the VA Requires to Approve PTSD
To grant service connection for PTSD, the VA requires three elements. Missing any one of them can result in a denial.
A DSM-5 PTSD Diagnosis: You must have a formal DSM-5 diagnosis, ideally from a licensed psychiatrist or psychologist. Diagnoses from mental health specialists carry the most weight in VA claims.
Proof of an In-Service Stressor: Proof that a traumatic event that occurred during military service. This can be combat-related (firefights, IEDs, rocket attacks) or non-combat-related (assaults, training accidents, medical trauma, or witnessing death).
A Medical Nexus: medical opinion stating that your PTSD is at least as likely as not caused by the in-service stressor. This link is what legally connects your diagnosis to service.
When VA Exam Already Satisfies the Nexus
In most PTSD claims, the VA orders a Compensation & Pension (C&P) exam with a VA or VA-contracted psychiatrist or psychologist. This exam is used not only to confirm a PTSD diagnosis, but also to establish the medical nexus.
If the examiner diagnoses PTSD and states that the reported stressor is adequate and related to the veteran’s symptoms, that opinion usually satisfies the nexus requirement on its own.
Who is Qualified to Write a PTSD Nexus Letter?
Most PTSD nexus letters should come from a mental health specialist, not a primary care provider. The right provider understands trauma, VA standards, and how to clearly connect your condition to service.
Psychologist/Psychiatrist (Strongest Option)
The best option for a PTSD nexus letter is a psychologist or psychiatrist. These specialists know how to evaluate trauma-related conditions and understand how PTSD develops over time. Their opinion will carry the most weight with the VA.
While scheduling or cost could be hurdles, their expertise makes their evaluation far more effective for supporting your claim.
Licensed Therapist or Counselor (Acceptable Backup)
If you can't get a letter from a psychologist or psychiatrist, a licensed therapist or counselor can be a solid backup — especially if you've been seeing them consistently over the years.
They can provide insight into your long-term symptoms, treatment progress, and how PTSD has messed with your daily life.
While their nexus letter might carry slightly less weight, their firsthand knowledge of your condition can still make a real difference in your claim.
Why Primary Doctors Are Usually the Wrong Choice
Primary care providers usually aren’t the right choice for writing a PTSD nexus letter, even when they know you well.
They typically don’t specialize in trauma-related mental health conditions
They aren’t trained to apply DSM-5 PTSD criteria
Their opinions often carry less weight with VA raters
That said, your PCP can still play an important role by documenting your symptoms over time and providing medical history that a specialist can reference in a strong nexus letter
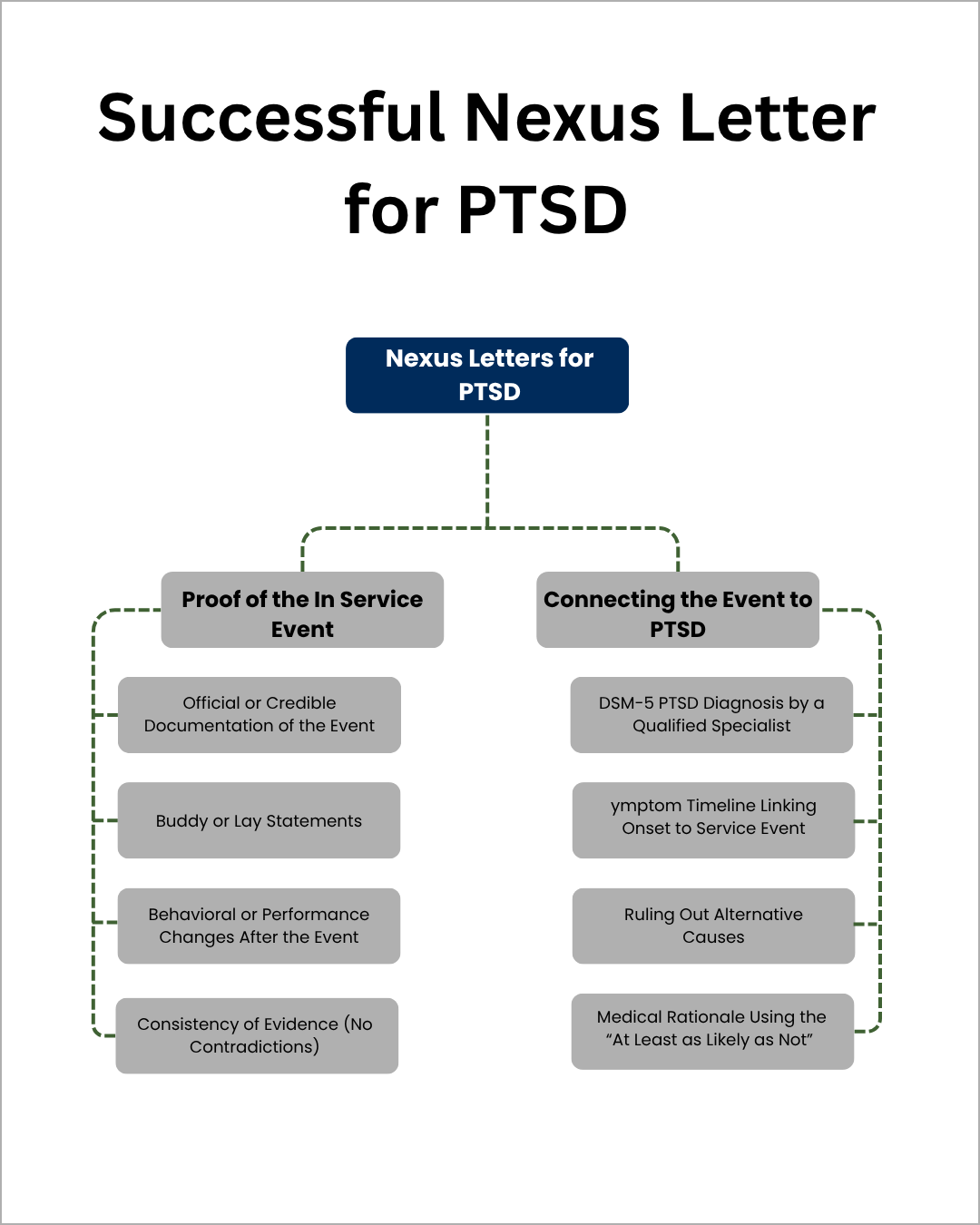
What Makes a Nexus Letter for PTSD Strong
Before you ask a doctor to write your letter, you need to be deeply familiar with what a nexus letter is and how it works.
Give your doctor this checklist before they write it, and review the letter carefully yourself before submitting it.
Common VA Examiner Objections Your Letter Must Address
Remember, your nexus letter must address any prior C&P exam. Claims are often denied when a medical opinion fails to address a C&P exam.
No DSM-5 PTSD Diagnosis: A nexus letter should clearly document a DSM-5–compliant diagnosis from a qualified mental health specialist.
The Veteran’s PTSD Was Caused by Something Else: VA examiners often cite childhood trauma, civilian stressors, or substance use.
Delayed Onset of Symptoms: If symptoms appeared years after service, the nexus letter should explain how delayed-onset PTSD commonly occurs
Non Combat Stressors Don’t Cause PTSD: This is a common examiner objection, make sure your nexus letter explains why these still fit the criteria for PTSD.
Understanding the specific issues examiners cite tells you the most important points to address.
Clearly Documenting When Symptoms Started and Progressed
When preparing your nexus letter, be clear and specific about your symptom history. The VA looks for consistency over time — not short spikes that disappear. Use this checklist to organize your information:
When symptoms began: Ideally within one year of discharge. If onset occurred later, your doctor must explain why and how this delayed onset developed.
Severity: Describe how symptoms impacted your daily functioning (sleep, work, relationships).
Progression: Note how symptoms worsened or changed over time, supported by medical or therapy records.
If your service records don’t fully capture your timeline, buddy or lay statements can fill those gaps.
These statements serve as credible secondary evidence showing the continuity of your symptoms after service.
Ruling Out Non-Service Causes of PTSD
This is where many PTSD nexus letters fall short. The provider must explain why your PTSD isn’t caused by something else — like preexisting conditions or post-service events.
The letter should:
Acknowledge any prior medical or mental health history
Explain why those earlier issues did not cause or contribute to current PTSD
Emphasize how military service directly worsened or triggered symptoms
Example:
“While the veteran experienced mild anxiety before enlistment, the frequency and intensity of night terrors increased dramatically following the 2008 blast exposure, indicating aggravation by military service.”
Doctors often forget to include this reasoning, and the VA assumes another cause — leading to a denial.
Medical Reasoning that Meets VA Standards
This is the most important part of the nexus letter — the medical logic connecting your PTSD to your service.
The provider must explicitly write:
“It is at least as likely as not (50% or greater probability) that the veteran’s PTSD was caused by, or aggravated by, their military service.”
That single sentence carries enormous legal weight.
Without it, the VA can’t legally grant service connection — no matter how strong the rest of your evidence is.
To make it stronger, apply the “1:1 rule”: Every factual statement in the letter should be backed by a piece of supporting evidence — a record, date, or observed symptom
How to Get a Nexus Letter for PTSD (Step By Step)
Finding the right doctor to write your letter takes time, and you may need to contact multiple providers before you get a yes. S
tart with free options through the VA and VSOs, then use local directories, and only consider paid companies as a last resort.
Step 1: Use Free VA and Community Resources First
Begin at your local VA medical center. VA doctors rarely write nexus letters, but they can still point you towards qualified providers.
When you call or visit, ask for a social worker or mental health case manager and explain that you're looking for community providers who handle VA disability evaluations.
Pro tip: You're more likely to succeed if you phrase it as a "medical opinion connecting your condition to PTSD" instead of a "nexus letter". People often get confused by that term and might not want to deal with it.
Step 2: Find Qualified PTSD Specialists Locally
If the VA can’t help, search Psychology Today or your state licensing board for providers specializing in PTSD, veterans, or forensic evaluations.
On Psychology Today:
Get Help → Talk to Someone → Find a Psychiatrist/Psychologist, then search your city or state.
Prefer profiles with:
MD/DO (Psychiatrists) or PhD/PsyD (Psychologists)
Mentions of PTSD, veterans/military, or disability evaluations/IME reports
Forensic psychologists are often best — they’re familiar with legal-style documentation like nexus letters.
Step 3: Ask VSOs for Recommendations
Veteran Service Organizations (VSOs) often maintain lists of trusted providers who understand VA standards.
Try:
Disabled American Veterans (DAV)
Veterans of Foreign Wars (VFW)
American Legion
A quick call can get you referrals to doctors experienced in VA evaluations.
Step 4: Research Paid Companies (last resort)
If you can’t find a local provider, some companies specialize in nexus letters — but quality varies dramatically.
Before paying, make sure to:
Verify credentials: Get the full name, license number, and specialty of the letter writer.
Review sample quality: Letters should include detailed reasoning, not generic statements.
Check reviews carefully: Use veteran forums, Trustpilot, or Google; watch for fake 5-star reviews or “guaranteed approval” claims.
A good company can save you time, a bad one can waste money and hurt your claim.
Step 5: Get Your Provider a Detailed Template
Doctors often decline nexus letters because they’re complex and time-consuming. Writing a template is the single most important thing you can do to increase your chances of success.
Doing your own research not only takes some stress off your doctor's end, but also shows the VA your initiative and effort — which they love.
The template should include:
Relevancy of your medical information
VA specific language
How to phrase their reasoning
Keep it simple — you're not telling them what to write, just giving them the format that the VA recognizes.
For a more detailed explanation, learn how to get a nexus letter step by step to make sure your evidence meets VA standards
PTSD Nexus Letter Example (Annotated Breakdown)
This is a nexus letter example presents a fictional case of a veteran who experienced a serious training accident during basic training.
In this scenario, the veteran witnessed a live grenade malfunction, resulting in severe injuries to fellow trainees.
Dr. Jane Smith, PsyD – Licensed Psychologist
123 Main Street • City, State, ZIP
Phone: (555) 123-4567
Date: October 11, 2025
To Whom It May Concern:
I have evaluated and treated Sergeant First Class Michael Thompson for Post-Traumatic Stress Disorder (PTSD). I am a licensed psychologist with over 15 years of experience in trauma and stressor-related disorders.
Mr. Thompson’s PTSD diagnosis was confirmed using DSM-5 diagnostic criteria and documented on VA Form 21-0960P-3 (PTSD Disability Benefits Questionnaire). His symptoms include intrusive nightmares, avoidance behaviors, hypervigilance, irritability, and persistent negative mood and cognition.
Annotation: Listing symptoms directly from DSM-5 improves credibility and shows diagnostic alignment.
During basic training in 2008, Mr. Thompson was exposed to a live grenade malfunction during a supervised exercise. Several trainees sustained severe injuries, and he directly witnessed the event. This incident is recorded in his service treatment records (STRs) and supported by two buddy statements (VA Form 21-10210) submitted with his claim.
Annotation: Adding exact forms and evidence types signals strong documentary support.
Within weeks of the incident, he began experiencing nightmares related to the explosion, exaggerated startle response, and avoidance of training environments. These symptoms were noted in mental health clinic notes from Fort Benning (June 2008) and have persisted since that time.
Annotation: Linking symptom onset to dated records builds a clear nexus timeline.
I reviewed his entire C-file, service treatment records, prior VA mental health evaluations, and therapy progress notes (2020–2025). The continuity of symptoms from service to present day demonstrates a direct and ongoing connection to the in-service trauma.
Other potential causes for his symptoms were carefully ruled out. He has no documented pre-service psychiatric history, no traumatic brain injury, and no non-service trauma that could explain his condition. He also denies substance abuse or other lifestyle factors that might contribute to his PTSD.
Annotation: Eliminating other possible causes strengthens the “at least as likely as not” standard.
Based on my review and clinical evaluation, it is my professional opinion that Sergeant First Class Michael Thompson’s PTSD is at least as likely as not (50% or greater probability) caused by or aggravated by his military service, specifically the 2008 live-grenade training accident.
This opinion is rendered using the VA’s “at least as likely as not” evidentiary standard and is supported by objective documentation, consistent symptom presentation, and the absence of alternative explanations.
Annotation: Restating the VA standard verbatim ensures the letter meets adjudication requirements.
Sincerely,
[Signature]
Dr. Jane Smith, PsyD
Licensed Psychologist
This example is longer than what most veterans expect, but that’s intentional — the VA looks for detailed, well-supported letters that clearly connect your condition to your service.
This sample is for educational purposes only and should not be used as an official medical or legal document.
Key Takeways: How to Strengthen a PTSD Claim
Navigating a PTSD claim with the VA can feel overwhelming, but a well-prepared nexus letter can make all the difference.
Whether you’re dealing with a non-combat trauma, a secondary PTSD claim, or an unfavorable C&P exam, the right letter connects your condition directly to your service and strengthens your case.
By understanding what the VA expects, finding the right provider, and ensuring your letter includes clear medical reasoning, you can give your claim the best chance of success.
Remember, a nexus letter is not just a form — it’s the key piece of evidence that turns your service and experiences into a compelling, service-connected claim
FAQ
-
You can get a higher VA rating for PTSD if your symptoms have worsened or if you are claiming that your PTSD caused another condition. Secondary conditions can include hypertension, sleep apnea, or migraines. In both cases, a nexus letter is needed to show the connection to your service-related PTSD
-
A 70% PTSD rating generally means your condition causes occupational and social impairment with deficiencies in most areas. This can include trouble completing tasks at work, difficulty maintaining relationships, periods of near-continuous depression or anxiety, and trouble handling stress. You might also experience withdrawal from family or friends, flattened affect, or occasional suicidal thoughts. The key is that your symptoms seriously disrupt most areas of your life, even if they aren’t constant
-
Denials usually happen if another condition or life event is seen as the main cause of symptoms, or if a C&P exam is unfavorable. A strong nexus letter and supporting documentation are usually the key to avoiding these issues
-
PTSD is diagnosed when a veteran has been exposed to a traumatic event and experiences symptoms like intrusive memories, avoidance, negative mood changes, or hyperarousal. These symptoms must last more than a month and cause significant problems in work, relationships, or daily life