How to Win a Sleep Apnea VA Claim in 2026: Step by Step Guide
Sleep apnea is one of the most heavily denied VA claims, even for veterans who do everything right. Many gather medical records, research studies, and service documentation only to get denied for vague or inconsistent reasons.
The real issue isn’t the diagnosis. It’s that the VA rarely connects sleep apnea to service unless the evidence is organized perfectly.
Most veterans never had a sleep study on active duty, and C&P examiners often blame factors like weight gain, lifestyle factors, or “no documented symptoms.” Without a clear timeline and strong medical link, the claim starts at a disadvantage.
I’ve helped many veterans win their sleep apnea claims and appeals, and the difference almost always comes down to documenting the timeline, choosing the right secondary connection, and presenting the medical evidence correctly from the start.
In this guide, I’ll show you the exact strategy veterans use to finally get approved—what the VA looks for, what actually proves service connection, and what mistakes lead to fast denials.
Understand the Two Paths to Winning a Sleep Apnea VA Claim
Sleep apnea claims are challenging, but they follow the same basic rule as any VA claim: the VA will grant service connection if you can prove it’s related to your service.
Veterans are also over twice as likely to develop sleep apnea than the general population, but the VA still does not list it as a presumptive condition under the PACT Act, Gulf War rules, Agent Orange exposure, or other common military hazards.
Because it isn’t presumptive, the VA won’t assume sleep apnea is service-related. To win direct service connection, you would need a documented sleep study or clearly recorded symptoms during active duty — something most veterans don’t have.
For that reason this guide focuses on the path that actually works for most veterans: secondary service connection, where a service-connected condition causes or aggravates your sleep apnea.
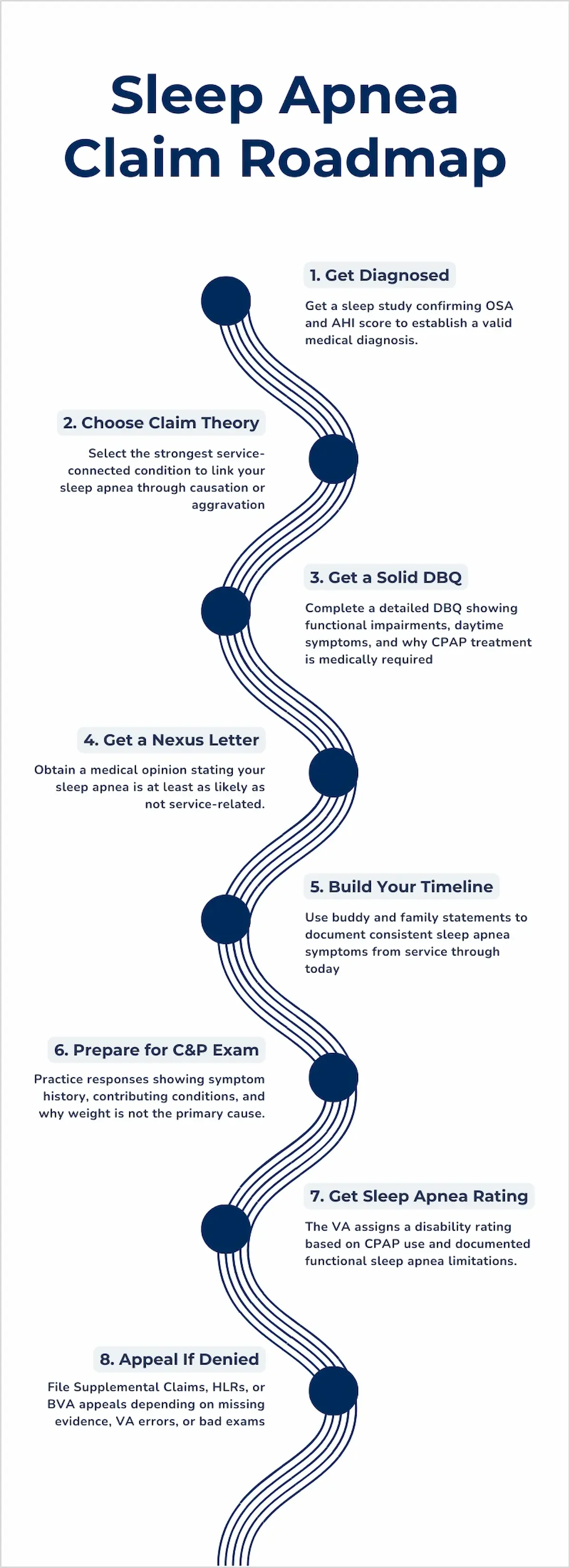
Step 1 — Get a Real Sleep Apnea Diagnosis
You cannot win a VA sleep apnea claim without a formal diagnosis from a sleep study. The VA requires an AHI score and medical interpretation before they can legally grant service connection.
OSA is the most common type in veterans and is approved the most. CSA and mixed sleep apnea can still qualify, but I won’t cover them here because they’re much harder to win and require significantly more evmaidence.
Choose the Right Sleep Study to Support Your Claim
There are two ways to get tested for sleep apnea: a home sleep study or a VA-ordered study. Both work as long as they include:
AHI score
Type of apnea (OSA, CSA, or mixed)
Interpretation from a licensed professional
VA Home Sleep Tests (HSTs) are common and much faster to obtain.
Private studies are often even quicker and can strengthen your claim if the VA is slow scheduling you.
The VA does not require the sleep study to be VA-issued, only that it’s legitimate and diagnostic.
Use Your AHI Score to Strengthen Severity and Rating Evidence
Your sleep study will show an Apnea-Hypopnea Index (AHI) score:
5–14 = Mild OSA
15–29 = Moderate OSA
30+ = Severe OSA
Important: AHI levels describe severity — they do NOT prove service connection. They are mainly useful for establishing a diagnosis with a measurable severity.
Know When You Actually Need a Second Sleep Study Before Filing
Most of the time, you only need one sleep study. The VA rarely orders a second sleep study unless:
Your previous study is very old
The documentation is incomplete
There is conflicting medical evidence
Even in these cases, C&P exam will likely still be scheduled, but it is not another sleep study and I will cover details on it later on
Step 2 — Choose the Condition You’ll Link Sleep Apnea to
Most veterans win through secondary service connection, meaning a service-connected condition caused or aggravated their sleep apnea. Choosing the strongest medically supported link dramatically improves your chances of approval.
Pick a Secondary Condition With Proven Medical Links to Sleep Apnea
Here are the strongest secondary links from my experience:
Sleep apnea secondary to PTSD: PTSD often causes sleep apnea through medication-related weight gain and disrupted sleep.
Sleep apnea secondary to asthma: Asthma and respiratory issues can narrow or inflame the airway, worsening sleep apnea.
Sleep apnea secondary to traumatic brain injury (TBI): TBI can disrupt the brain’s breathing regulation, leading to sleep apnea.
Avoid Weak Secondary Links Unless You Have a Very Strong Case
Other links exist, such as sleep apnea secondary to tinnitus, GERD, orthopedic pain, or medication side effects.
However, these are approved far less often and typically require a much more detailed medical rationale.
Unless you are thoroughly educated and have overwhelming evidence, I recommend that you avoid them.
Step 3 — Complete a Strong Sleep Apnea DBQ
A detailed sleep apnea DBQ shows the VA how severe your symptoms are and how they affect your daily functioning. Strong DBQs document real-life limitations and clearly explain why a CPAP was prescribed.
Document Daily Functional Impairments That Increase Your Rating
Your DBQ needs to show measurable, real-life examples of how your symptoms limit you. Generic statements like “sleep apnea affects my life” are not helpful.
Ask your doctor to document these five symptoms on your DBQ:
Difficulty staying awake while driving
Trouble concentrating at work
Excessive daytime fatigue affecting job performance or relationships
Waking up unrefreshed, irritable, or mentally foggy
Needing naps or falling asleep unintentionally
You can also briefly clarify how your symptoms differ from other conditions like narcolepsy or hypersomnia, which involve uncontrollable sleep episodes.
If you experience sleep disturbances, such as frequent awakenings, gasping, choking, or restlessness, make sure your provider documents them.
Strong DBQs don’t prove service connection but are important for getting a rating.
Show Why You Need a CPAP (Not Just That You Have it)
If you use a CPAP machine, your doctor must explain:
Why you were prescribed it (e.g., moderate/severe AHI, oxygen desaturation)
How it improves your symptoms
What your sleep was like before treatment
Examples of strong CPAP-related statements:
“CPAP reduced his nighttime choking episodes.”
“He wakes more rested with CPAP but still experiences significant daytime fatigue.”
“Without CPAP, he cannot maintain adequate oxygen levels during sleep.”
Do NOT write a DBQ that just says “Veteran uses a CPAP.” The VA needs to know why it was prescribed and how severe your symptoms were without.
Step 4 — Prove Service Connection (This is What Actually Wins Your Case)
To win a VA sleep apnea claim, you must prove service connection. This usually requires a nexus letter explaining how a service-connected condition caused or aggravated your sleep apnea
Use a Nexus Letter to Establish Causation or Aggravation
The VA rarely establishes this link on its own, which is why most veterans need a strong nexus letter for sleep apnea.
A nexus letter is the single most important piece of evidence for most sleep apnea claims. It explains why your service-connected condition caused or aggravated your sleep apnea
A nexus letter:
Gives the VA the medical reasoning required for approval
Supports well-documented secondary links
Helps prevent examiners from defaulting to denial
Choose Whether Your Claim Is Based on Causation or Aggravation
Sleep apnea can be linked secondarily through either causation or aggravation, and you must clearly identify which applies to your claim.
Causation (Direct Cause): Your service-connected condition led to the development of sleep apnea.
Example phrases:
“PTSD caused chronic sleep fragmentation that contributed to OSA.”
“Chronic sinusitis created nasal blockage leading to airway collapse.”
“Asthma caused nighttime airway inflammation contributing to OSA.”
“Service-connected medication caused weight gain that led to OSA.”
Aggravation (Made It Worse): Your service-connected condition worsened an existing or developing sleep apnea condition.
Example phrases:
“PTSD increases nighttime arousals, worsening OSA severity.”
“Rhinitis episodes block nasal airflow, aggravating apnea events.”
“TBI disrupts sleep regulation, increasing breathing interruptions.”
“Medication-related weight gain aggravated the veteran’s OSA.”
You must clearly state whether you’re claiming causation or aggravation because the VA may not infer it for you. Failing to do so will likely lead to denial.
Need Help With Your VA Claim?
Speak with a VA claims specialist to understand your options and next steps.
Call 888-820-8520Step 5 — Strengthen Your Timeline with Testimonial Evidence
Timeline evidence from buddies, spouses, or family members helps show when your symptoms began and how they progressed. These statements fill gaps in medical records and make your claim more believable to VA raters.
Buddy Statements From People Who Served with You
Sleep apnea symptoms often go unnoticed during service, but your fellow service members may have seen or heard things you didn’t recognize as apnea-related. Remember, symptoms often occur long before a diagnosis.
Useful examples include:
Loud, chronic snoring
Excessive fatigue during PT or daily duties
Falling asleep unintentionally
A strong buddy statement simply describes what they witnessed, not medical conclusions.
Example: “During deployment in 2012, I shared a room with the veteran. I frequently heard him stop breathing in his sleep and wake up gasping for air.”
Lay Statements From Spouses or Family
Lay statements serve a different purpose than buddy statements. While they can describe similar symptoms, their main value is showing how your sleep apnea changed over time.
Family members can document:
What your sleep looked like before CPAP
What improved after starting CPAP
What symptoms still remain
How your sleep apnea affects daily functioning or relationships
Example: “Before he started using CPAP, he would choke or stop breathing several times a night. The CPAP has reduced the choking episodes, but he still wakes up tired and struggles to stay awake in the afternoons.”
What Makes a Timeline Credible to the VA
A credible timeline shows your sleep apnea symptoms were consistent and observable over time, even if you can’t remember exact dates. The VA is looking for patterns, not perfection.
A strong timeline includes:
Specific time periods (“During deployment in 2014…”)
Firsthand observations (not medical opinions)
Clear examples of symptoms (snoring, choking, gasping, daytime fatigue)
Multiple statements that align with each other
Consistency with medical records and CPAP notes
If your sleep study happened soon after leaving service, timeline matters less since the VA already sees a close connection. Regardless, testimonial evidence still helps document symptom severity, which you need to get a high rating.
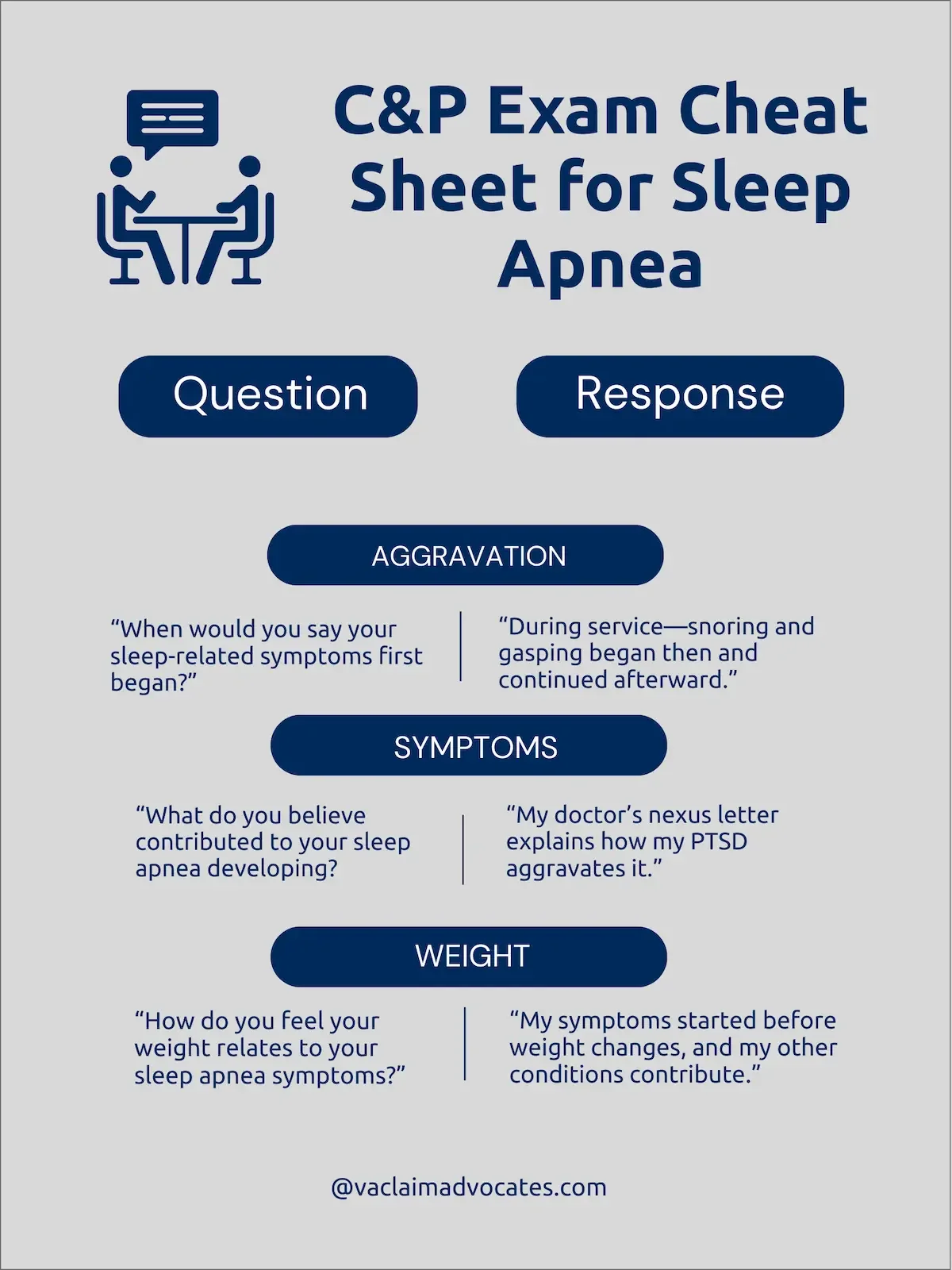
Step 6 — Prepare for C&P Exam
The C&P exam often decides the entire claim, so how you answer common questions matters. Clear, consistent explanations help address examiner concerns about onset, contributing factors, and weight.
You should never argue with the examiner, but you should phrase your responses in a way that subtly addresses their typical concerns. Here are some examples:
Give Detailed Answers to Symptom Onset Questions
The examiner will ask you exactly when your symptoms began. Here’s a good answer:
Response: “My symptoms began during service, like loud snoring and waking up gasping, one of my fellow service members brought it up to me, but I was not evaluated. They continued after service and gradually worsened.”
(Preempts: “no sleep study in service”)
Why it works: This response clearly explains when the symptoms began and points to a buddy statement that supports the timeline.
Explain Contributing Factors Without Hurting Your Claim
Make sure the examiner knows that other factors exist, but point to evidence on why they can’t be the only explanation.
Response: “My doctor explained in the nexus letter that my PTSD/asthma/rhinitis can aggravate or contribute to sleep apnea. He cited medical literature showing how these conditions affect breathing and sleep quality, which is why he believes they played a role in my case.”
(Preempts: “no medical link” and ignoring aggravation)
Why it works: This response acknowledges that weight may be a factor, but makes it clear it isn’t the only cause of his sleep apnea.
Address Weight Gain Carefully to Prevent an Automatic Denial
Weight gain is the most common objection you will get from examiners, and you need to address it carefully:
Response: “My symptoms started before any weight gain, and my service-connected conditions contributed to those changes. So weight may play a role, but it isn’t the only factor affecting my breathing or sleep.”
(Preempts: “obesity is the primary cause”)
Why it works: The doctor also addressed weight, explaining that while it may contribute, it is not the only factor—an essential clarification, since blaming obesity is the single most common reason sleep apnea claims get denied
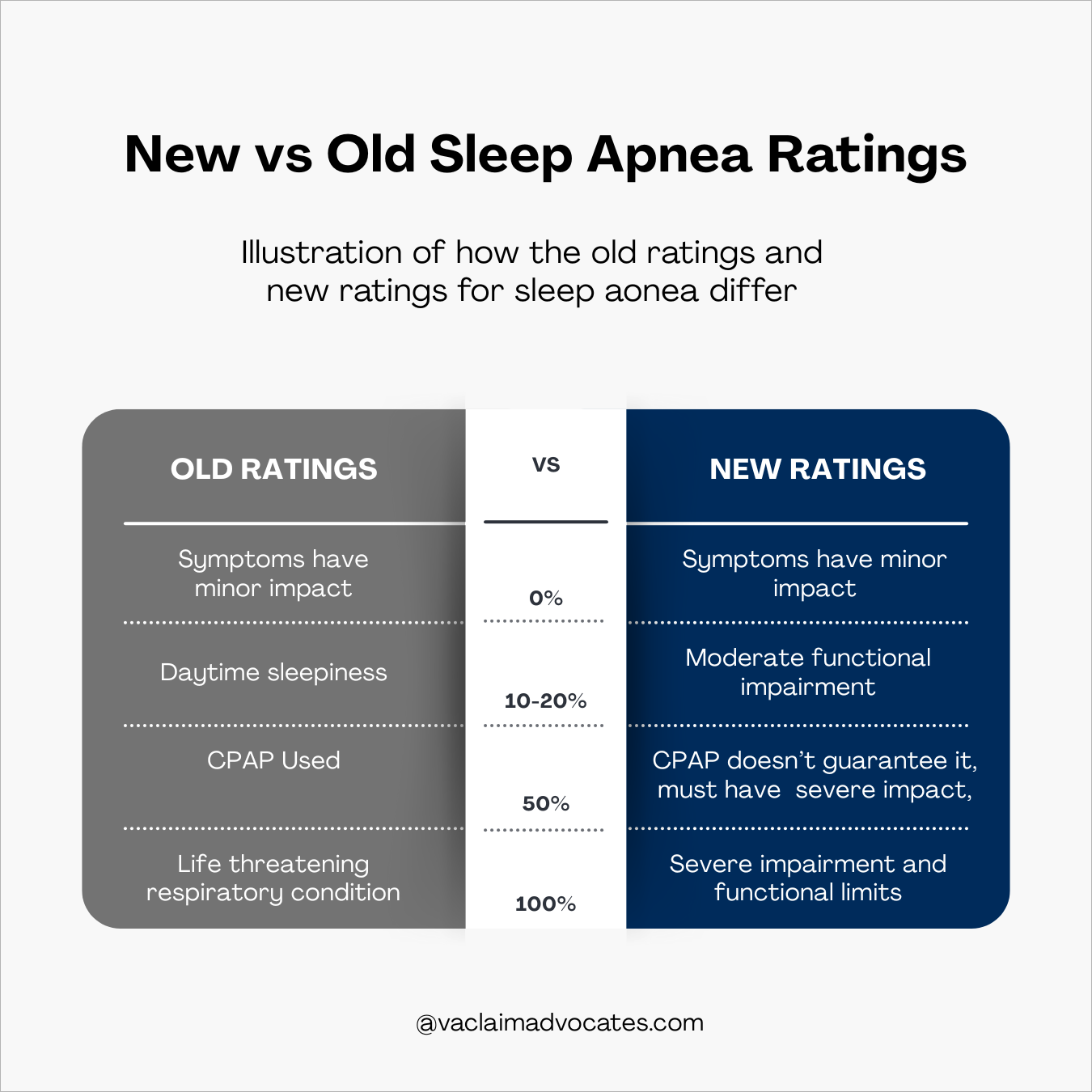
Step 7 — Understand How the VA Rates Sleep Apnea
The VA currently awards a 50% sleep apnea rating for CPAP use, but upcoming rule changes will shift ratings toward functional impairment instead. Filing before the new rules take effect can lock in a higher rating for life
Know What the New Proposed Rating Rule Means for You
Under the current (old) rating criteria:
Being prescribed a CPAP automatically qualifies you for 50%.
Under the proposed rule changes:
CPAP use no longer guarantees a 50% rating
Many veterans with well-controlled sleep apnea may receive 0–10%
Ratings will focus on functional impairment, not just device use
The VA will evaluate how sleep apnea affects your daily life, including fatigue, concentration, and safety
This means simply having sleep apnea is not enough — you must show how severely it impacts you, even with treatment.
See How Sleep Apnea is Rated Today Under 38 CFR 4.97
The current Diagnostic Code 6847 assigns:
50% for veterans who require CPAP
30% for persistent daytime fatigue
0–10% for well-controlled or mild symptoms
These are the rules most veterans want to stay under because they award compensation more generously.
AHI levels (mild, moderate, severe) do not determine the rating — functional symptoms do.
File Before the Rule Change if Possible
If you file before the rule change, you stay under the current criteria for life.
This is called being “grandfathered in,” and the VA cannot switch you to the new system later.
If you file after the rule change, you will be rated under the new criteria, which heavily emphasize functional limitations and quality-of-life impact.
Step 8 — Appeal the Decision if You’re Denied
If denied, the VA appeal path you choose should match the reason for the denial. Supplemental Claims help missing evidence, HLRs correct VA errors, and Board appeals challenge flawed exams or complex medical issues.
File a Supplemental Claim Only When You Have Strong New Evidence
Make sure the new evidence you plan to submit is not only new but also relevant. The VA will deny a Supplemental Claim if the additional evidence does not directly address the reason your claim was denied in the first place.
File a Supplemental Claim (VA Form 20-0995) when your evidence was incomplete, weak, or missing. This is the right choice if you were denied because:
You didn’t submit a VA nexus letter
The nexus letter lacked medical rationale
Testimonial evidence didn’t clearly describe symptoms or timeline
Your DBQ didn’t document severity or CPAP use
In these cases, the VA didn’t necessarily make an error — the evidence simply wasn’t strong or specific enough.
Supplemental Claims rarely overturn a negative C&P exam because VA raters give more weight to the examiner’s opinion than to newly submitted evidence, even when it is medically stronger.
Request a Higher-Level Review When the VA Got It Wrong
File an HLR when you did submit strong evidence, but the VA misinterpreted or ignored it.
Common errors include:
Ignoring a nexus letter that clearly explained causation or aggravation
Overlooking aggravation entirely
Misreading your DBQ (very common for sleep apnea)
Dismissing testimonial evidence without explanation
Giving too much weight to a flawed C&P exam
One of the most common HLR scenarios is Sleep apnea denied secondary to PTSD. This is often due to examiners falsely claiming “no medical link.”
An HLR (VA Form 20-0996) puts a senior rater on your claim. You cannot submit new evidence, but the reviewer can overturn the decision if the VA made an error.
Take Your Case to the BVA for the Highest Chance of Reversal
In some cases, the VA can deny claims despite strong nexus letters and other supporting evidence.
Both the Supplemental Claim and HLR failed
You need a doctor’s testimony or additional medical opinion
You believe the C&P exam was deeply flawed
The case requires a judge to weigh competing medical opinions
The Board takes longer, but it gives you the best chance to challenge a bad C&P exam or a repeated VA misinterpretation.
I've seen many sleep apnea secondary claims receive the fairest and most thorough review at the Board of Veterans’ Appeals. It takes longer, but Board judges are more willing to weigh medical evidence, consider aggravation, and challenge weak C&P examiner opinions.
Final Thoughts on Winning Sleep Apnea Claim
In the end, winning a sleep apnea claim comes down to building a clear, well-supported connection between your condition and your service or another service-connected disability.
Make sure your timeline is easy to follow, your medical evidence is thorough, and your lay statements back up your story with credible, firsthand details about how your symptoms developed and affect your daily life.
The stronger and more consistent your evidence is, the harder it is for the VA to deny your claim.
Take the time to organize everything clearly and don’t be afraid to seek help if you need it — doing so can make the difference between a denied claim and the benefits you’ve earned.
FAQ
-
To file a claim for sleep apnea, submit VA Form 21-526EZ online through VA.gov, by mail, or in person at a VA regional office. Include medical records, a sleep study confirming the diagnosis, and any evidence linking it to your service or a service-connected condition
-
While it’s technically possible to fail a VA sleep apnea test by staying awake, using stimulants, or altering your sleep habits before the study, doing so is strongly discouraged. These actions can lead to inaccurate results, delay your diagnosis, and hurt your claim. It’s always better to be honest and let the test reflect your true condition so you can receive the proper care and benefits
-
The VA is changing the way it rates sleep apnea, which will be based on how severe it is and how much it impacts your daily life. Ratings range from 0% if it’s diagnosed but causes no symptoms, up to 100% if it results in chronic respiratory failure or requires a tracheostomy. Most veterans who use a CPAP machine receive a 50% rating
-
the best approach I found is through a secondary service connection. What you're basically doing is showing that another service-related condition—like PTSD, rhinitis, or sinusitis—actually caused or contributed to your sleep apnea. Trust me, this connection can make all the difference in getting your claim approved.
-
several medical conditions are commonly connected to sleep apnea. The big ones include PTSD, chronic rhinitis, sinusitis, obesity, hypertension, and heart disease. For us veterans especially, sleep apnea claims often work best when they're filed as secondary to PTSD or respiratory issues that developed during service. The connection between these conditions and sleep apnea is well-documented, which definitely works in your favor when building your case.